The Covid-19 pandemic has been a great source of fear and trepidation for the population since it began to circulate around the globe in early 2020. As news began to spread about how this virus could infect anyone, regardless of any pre-existing conditions, body type, physical shape, or overall health, the science explained that no one is any more likely to become infected based on any other health concern than anyone else.
As time passed and clinical studies of Covid-19 began to take place, a startling revelation came to light: Certainly, anyone could be infected by the disease, however, for those who live with obesity, the outcome from the infection can be much more severe, and possibly life-threatening.
Obesity and COVID-19: Chronic inflammation leads to Hospitalization
Chronic inflammation is a condition that those with obesity often live with, as conditions that stem from obesity such as high cholesterol, diabetes, heart disease, and sleep apnea are associated with the inflammation of many of the core systems that support body function.
Recently a CDC study that examined patient data taken from COVID-19 patients reported that patients who suffer from underlying health conditions such as the ones stated above are more than six times more likely to be hospitalized, five times more likely require ICU admission during that hospitalization, and a staggering 12 times or higher more likely to die from the disease than those who do not suffer from chronic inflammation.
Obesity is not simply the cause of more severe symptoms in this case; it will also complicate the treatment process, leaving those who are currently living with obesity much more susceptible to deeply complicated recoveries and persistent health issues after you recover.
For those who suffer from pulmonary hypertension, cardiovascular disease, narrowed blood vessels, or pre-existing lung damage, the responsiveness to a ventilator during treatment is often greatly decreased, complicating both initial treatment and recovery efforts. Ultimately, the only way to avoid these complications due to obesity is to adopt healthier habits that will lead to weight loss.
Obesity and COVID-19: Outcomes Worsen for Obese Patients

Adults who experience obesity have a much greater risk of negative persistent outcomes for those who are infected by COVID-19. Historically, obese patients pick up underly medical conditions as their body is working under difficult circumstances that affect important systems in the body. Prior to COVID-19, patients suffering from obesity already had an increased chance of being negatively affected due to the excess strain on the body attempting to normalize functions of internal organs already being limited due to conditions such as heart disease, diabetes, high cholesterol amongst others.
When the body of an obese patient begins to be affected by COVID-19, the risks and severity of the effects of the virus are increased. Patients who suffer from obesity also face an increased risk of hospitalization after contracting the disease by triple. This is due to a marked decrease in immune function that most sufferers of obesity have as a preexisting condition to being infected with COVID-19. One of the most dangerous preexisting conditions that Obese patients exhibit and are exacerbated by the virus is decreased lung capacity. During treatment for COVID-19, the decrease in total capacity, as well as a decrease in a reserve capacity, make it very difficult for those hospitalized patients to receive adequate ventilation during treatment. Another difficulty for those obese patients suffering from COVID-19 is a lower response to vaccines for the disease, as is demonstrated from a low response to numerous other diseases such as Hepatitis B, tetanus, and certain strains of influenza. One of the most important ways an obese person to fight the disease before they are infected is to attempt to lose weight and mitigate preexisting health conditions that will cause more difficulty to the patient both when
Improve Your Health Naturally

Quarantine, isolation, and pandemic based anxiety has created an incredibly stressful environment for everyone. Often times this stress and anxiety will lead to eating more as a coping mechanism, exacerbating poor eating habits and food choices, leading to an even more difficult issue to address.
Obesity is an incredibly complex disease that is influenced by a number of contributing factors outside of caloric intake that decreases the chances of a patient finding an easy path to correct the disease. Factors such as neighborhood location, access to affordable, healthy food, as well as access to safe and convenient places for exercise all contribute and impact those with obesity. Underlying societal and systemic determining factors often deeply affect those with Obesity making it more difficult for patients who suffer from the condition to receive proper guidance and management skills for affliction. Unfortunately, these same disparities make it even more difficult for those who are already suffering from Obesity to receive outside care to support a healthier lifestyle that would mitigate the severity of COVID-19 infections. These disparities and the unfortunate circumstances that stem from them may affect individuals who are seeking treatment and vaccination from COVID-19.
Changing your habits at a systemic level takes time, especially when considering long-term weight loss strategies. However, there are a few steps Obese patients can take when attempting to decrease their weight and combat the negative health consequences that are inherent in those suffering from weight issues. Some of the best preliminary steps one can take are: Eating a healthy diet, being physically active, Sleeping Enough, and learning to deal with stress in healthy ways.
Eating a Healthy Diet

Consuming a diet that includes plenty of fruits and vegetables, lean and healthy proteins, and whole grains while keeping portion control and caloric intake in mind is incredibly important for your health and well being, as a proper diet can help with weight loss as well as contribute to keeping the weight off once it has been lost. Having good nutrition and fighting the conditional negative health complications of obesity will support proper immune function allowing for your body to be more prepared in the event of being infected with COVID-19. Lowering your total BMI will allow an obese patient to self treat health conditions such as heart disease and type 2 diabetes, which greatly increases the severity of a COVID-19 infection.
This situation can be improved by making healthier decisions about the food you eat, as well as forming healthier eating habits.
One of the best ways to improve your health naturally is to concentrate on eating well and changing your diet to one that is plant-based. Although it may seem difficult to move away from animal-based meals, there are many non-processed, non-meat based meals that remain delicious while encouraging weight loss.
When choosing an alternative diet that encourages weight loss, there are many options to consider. Some of the most important choices for a healthier diet include options that are:
High in Fiber: such as bran, lentils, avocado, or other foods that normalize your bowel movements and encourage the growth of bacteria in the gut which assist with cleansing your system of toxins.
Rich in Antioxidants: examples include fruits and vegetables such as raspberries, blueberries, kale, red cabbage, and spinach.
Vitamin-boosting foods: Foods that contain B vitamins, Potassium, Vitamin C, and Zinc such as beans, nuts, bananas, oranges, and peppers.
Beginning your weight loss journey through adopting healthier eating habits will certainly assist you in boosting your metabolism, as well as your overall health. One can also benefit from boosting their internal health by taking vitamins and minerals that will supplement the nutrients your body is already taking in from consuming healthier, unprocessed food.
Being Physically active

Adding regular exercise to your daily routine is another way that one is able to push themselves towards improving their health. Starting off slowly with a short walk and building up to more intensive workouts will also boost your metabolism and help you burn off excess calories. After higher metabolic function begins to increase metabolism, the body will adapt in order to process calories faster and with less stress on your body.
Regular physical exercise and activity will help anyone feel better, sleep more soundly, and reduce stress, however for those who suffer from obesity, this is especially paramount to a healthier lifestyle and better outcome when surviving COVID-19. When someone maintains a physical activity regime, the body is more capable of helping to prevent disease, due to the function of the body’s important systems working more efficiently and properly. Physical activity will also help to mitigate heart disease as well as type 2 diabetes, increasing obese patients’ chances of preventing catastrophic effects that could come from COVID-19, and boost a patient’s overall function of the immune system.
Sleeping Enough

Not getting enough sleep is one of the leading causes of emotional depression, as well as one’s susceptibility to chronic diseases. Sleep deprivation can also increase the severity of heart disease, type 2 diabetes, and obesity as a whole. When a person does not sleep long enough, the body is not afforded the amount of time and rest that is required for self-healing and proper function throughout the body. The less sleep one gets, the more likely one is to be afflicted by a number of chronic diseases, as well as a reduced immune system. For obese patients, this is especially important when attempting to rebuild one’s body into a healthy well functioning system. Getting enough sleep is one of the most basic ways for someone to boost their immune system as well as begin the journey towards weight loss.
If you get five hours of sleep or fewer on a regular basis, your body has a tendency to hold on to increased levels of visceral fat due to a stress mechanism that is hardwired into our brains. Not only will the added stress of depriving your body of the rest it so deeply needs to affect your emotional state, but it can also cause you to crave more sugary foods, as your body will desire boosts of energy to stay awake.
A good rule to go by is to set a regular sleeping schedule where you wake up and go to bed at the same time each night. This will increase the likelihood of your body becoming accustomed to a normal fat-burning cycle and will help regulate your metabolism, eventually leading to holding on to lower levels of body fat. Getting enough sleep and keeping a consistent sleep schedule should be a priority since it can affect not only your abdominal fat but your overall weight and health.
Coping with stress

The Pandemic is certainly one of the most stressful periods for anyone who is currently living through it, as the uncertainty of the future, job-related stress and uncertainty, and general concerns for the wellbeing of family and friends have caused deep stress and anxiety to afflict many during COVID-19. Unfortunately, stress, especially during a pandemic, can cause distressing changes in habitual behavior, as people attempt to cope with the onslaught of constant stress and concern. If stress is not mitigated, chronic health problems, a poor diet, and increased use of alcohol and tobacco will worsen chronic health problems and put the body at further risk of not being able to cope with physical issues, let alone the emotional stress that comes with it.
Surgical Weight Loss Options
For those who are living with obesity and truly want to lose weight, there are times when exercising and changing your diet will simply not be enough to achieve your weight loss goals.
The next step is to explore surgical weight loss options that will significantly improve your ability to lose weight.
Two of the most common surgical procedures that will assist in weight loss are gastric bypass surgery and gastric sleeve surgery.
Sleeve Gastrectomy Procedures
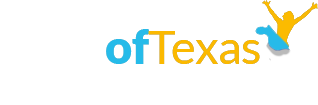
Sleeve Gastrectomy Procedures are less invasive than gastric bypass surgeries, as the surgeon reduces the size of the stomach by removing about 80 percent of the stomach capacity, and forming a banana-shaped sleeve that allows for a relatively normal digestive process.
Regardless of which procedure is performed, the reduced capacity of the stomach will cause the patient to lose weight more rapidly.
Sleeve gastrectomy is usually performed laparoscopically, with your doctor using tiny instruments through small incisions. About 75 percent to 80 percent of your stomach is removed during this weight loss surgery, leaving a banana-shaped pouch. Due to your stomach’s smaller size, you can expect to eat less food than you did prior to the procedure. This surgery may also reduce the amount of the hunger-stimulating hormone ghrelin produced by your stomach, resulting in a reduced appetite.
This type of weight loss surgery is simpler than a gastric bypass, and you’ll still absorb the normal amount of nutrients from the food you eat. However, you may need supplements since you’ll be eating less.
Who is a good candidate for a sleeve gastrectomy procedure?
You may be a good candidate for sleeve gastrectomy if your BMI is 40 or higher, which is classified as extreme obesity. If you have a serious health condition that’s related to your weight—such as type 2 diabetes, sleep apnea, or high blood pressure—you may be able to have a lower BMI of 35 to 39.9. More than 75 percent of people who have laparoscopic gastric sleeve surgery experience an improvement or even a reversal of these diseases.
Although Gastric Sleeve procedures are more popular due to the relative simplicity of the process in relation to Gastric Bypass, the more effective surgery, either of the procedures will immediately improve the amount of blood sugar in your body, allowing the body to combat diabetes more readily, allowing the body to process smaller amounts of the sugar more efficiently.
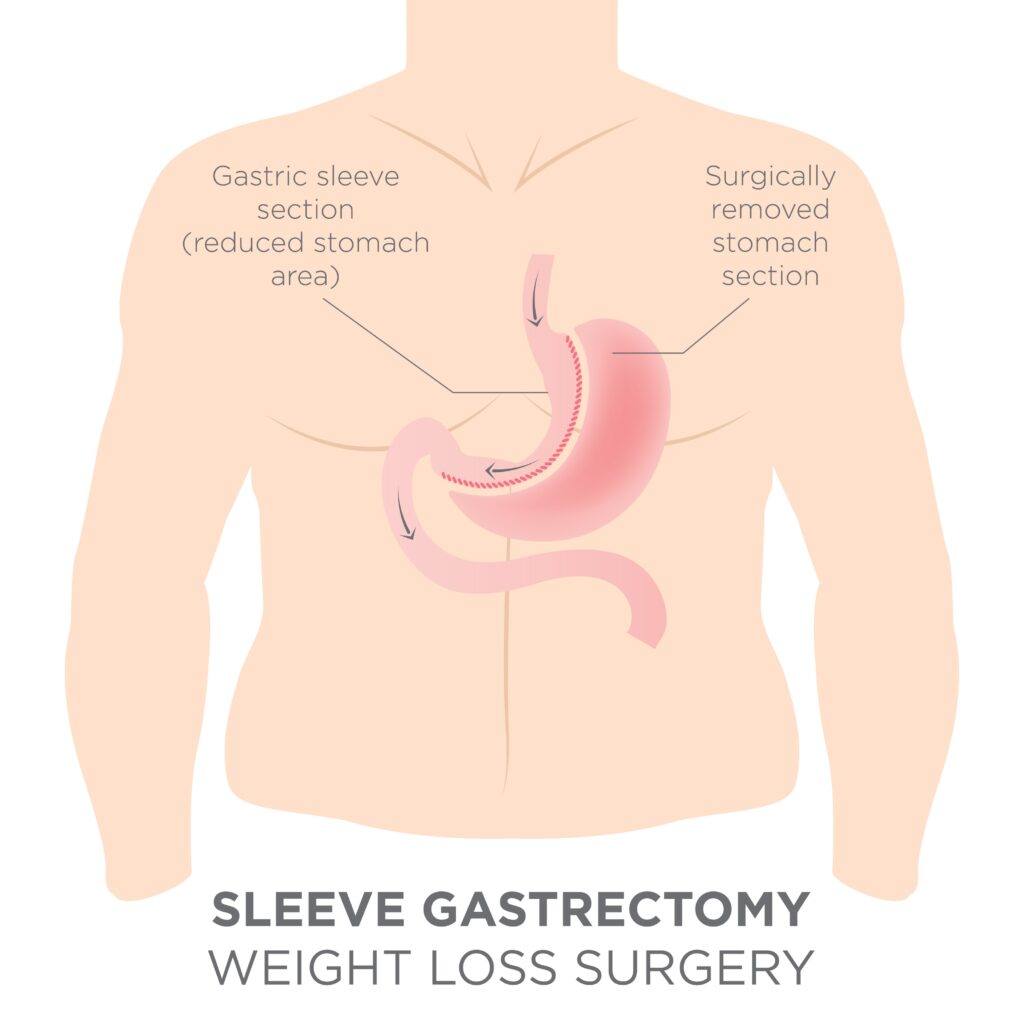
Gastric Bypass Surgery
Sleeve Gastrectomy Procedures involve creating a pouch at the top of the stomach that significantly reduces the physical size of the stomach through bypassing most of the stomach and surgically reconnecting the small bowel to a lower point in the digestive path. The reduced stomach size will immediately reduce hunger, as the patient’s stomach will fill up faster will less food. The body will then begin to increase metabolism and absorb nutrients faster in an attempt to catch up with the caloric intake that the body is used to.
Gastric bypass sometimes referred to as the Roux-en-Y gastric bypass, is a more complicated procedure than sleeve gastrectomy. The first stage of the surgery is like a gastric sleeve procedure and involves dividing the stomach, creating a small stomach pouch. The second stage involves working around the intestine—specifically, the first part of the small intestine is divided, and its bottom end is connected to your new, smaller stomach pouch. The divided small intestine’s top portion is then re-routed further down on the small intestine, which allows the first part of your small intestine to be bypassed so the stomach acids and enzymes will eventually mix with food lower down.
The procedure works by creating a small stomach pouch that holds far less food and it reduces the amount of ghrelin that your stomach produces. In addition, since a section of your small intestine is bypassed when you eat, you’ll absorb fewer calories and nutrients. You may be able to lose 60 percent of your excess weight—or more—in the two years after your surgery, and in general, gastric bypass patients tend to have a higher percentage of weight loss compared to those who undergo a gastric sleeve surgery. As a result of this surgery, you may experience “dumping syndrome,” which occurs when your food is moved from your stomach pouch directly into your small intestine without being digested. If this happens, you may need to change your diet or take prescription medicine.
Who is a good candidate for gastric bypass?
Gastric bypass is usually performed in obese patients who have a BMI of more than 45. In some cases, you can qualify for the procedure with a lower BMI if you have an obesity-related condition that may be improved by gastric bypass surgery.

Regardless of how your weight loss journey begins, the outcome of escaping obesity will positively impact the overall health of the body, as well as give those who were formally the most susceptible to complications from COVID-19 a much higher chance of surviving an encounter with the Coronavirus, and a brighter future after being exposed to the virus.
To find out whether weight loss surgery might be right for you—and if so, which one—contact BMI of Texas today. We’re happy to help you evaluate your options, giving you the insight you need to make an informed decision that will give you the best chance of weight loss success.